The human cost of organ scarcity is tragically real. In the United States alone, more than 100,000 patients wait for the possibility of an organ transplant. Every eight minutes, a new name joins the waiting list, while 17 die on the list each day—a stark reminder of the critical shortage and soaring demand for organs.
Not only is the demand overwhelming, but geographical limitations, short transport lifespans for organs, and strict donor criteria also restrict the pool of available organs. However, we’re on the brink of a breakthrough—not through a single revolutionary technology, but by optimizing what we already have.
Reforms in organ allocation, efforts to increase donor organ utilization rates, innovative surgical techniques, and advanced preservation technologies can—and have been proven to—collectively expand the pool of viable human organs.
We’ve only scratched the surface of what’s possible in optimizing human organ transplantation. Achieving a more equitable system and maximizing successful transplants requires a collective effort to ensure these advancements reach those who need them most.
Advanced Organ Preservation for a More Equitable System
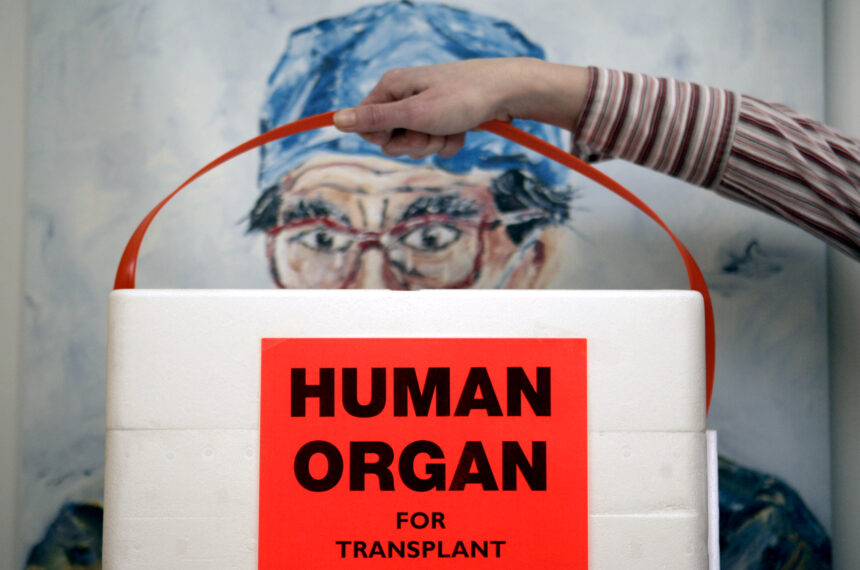
In the past, where you lived geographically significantly impacted your chances of receiving an organ transplant. Traditionally, organs were—and in some cases, are still—transported in commercial-grade coolers packed with ice, restricting the distance they could travel while remaining viable.
This outdated method has a critical flaw—ice damage. Transporting organs on ice exposes them to freezing temperatures, which can cause irreversible cellular damage and render them unusable. This tightens the window for transplantation and restricts the pool of compatible recipients to those geographically close to the donor. An organ available in California, even when flown by private charter, wouldn’t survive the journey to a recipient waiting in New York City.
New technologies and their adoption by the transplant and donation community have largely eliminated geography and distance as barriers to transplantation without sacrificing excellent clinical outcomes. Organs now routinely travel distances that span from Alaska to the East Coast.
Frank May/picture-alliance/dpa/AP Images
Advanced organ preservation technology, such as hypothermic preservation devices, ensures optimal conditions during transport. These specialized devices allow transport teams to track critical data, such as location, temperature, and pressure. The technology makes it possible to safely transport organs over longer distances and ultimately expand the pool of potential donors.
New Techniques Expand the Donor Pool for Transplants
Compounding the organ shortage are strict criteria for both usable organs and transplant eligibility. Only organs from specific donors, depending on the circumstances of death, are viable for transplant.
However, advanced methodologies and organ preservation technologies have established a new donor pool, enabling doctors to use organs from donors whose hearts have stopped beating—known as donation after circulatory death (DCD).
Traditionally, certain organs from DCD donors weren’t considered for transplantation. New technologies now allow DCD organs to be assessed before transplant. Machine perfusion uses specialized machines that mimic human body functions, keeping the DCD organ in a near-functioning state outside the body while it’s being assessed.
Significant developments are also being made in organ recovery using normothermic regional perfusion (NRP). Instead of fully removing the organs, surgeons can assess them within the deceased donor’s body.
Advancements like machine perfusion, NRP, and hypothermic preservation devices integrate with existing practices. These methods keep organs viable longer, while new preservation technologies extend travel distances. Together, these advancements are increasing the number of life-saving human organ transplants.
Making Use of Underutilized Human Organs
The utilization rate of consented organs for transplants remains quite low. Research found that often fewer than 30 percent of consented hearts and 20 percent of consented lungs are used. Optimizing the use of currently available organs, embracing new preservation technologies, and most importantly, equipping the organ donation community with the necessary resources and training to effectively implement these advancements must be a priority.
While the state of transplantation is not without challenges, we can address many of them with the technology we have today. We owe it to patients waiting for a second chance to build on our progress and achieve even more through ongoing research, innovation, and collaboration across the industry.
The organ transplant and donation community is already achieving clear and measurable success with existing advancements. Increasing the amount of successful transplants is achievable now, but it’s not going to be one technology or technique alone. We need widespread adoption of these innovations, involving clinicians, scientists, and patients alike.
Dr. Lisa Anderson is CEO and founder of Paragonix Technologies.
The views expressed in this article are the writer’s own.
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
“);jQuery(this).remove()})
jQuery(‘.start-slider’).owlCarousel({loop:!1,margin:10,nav:!0,items:1}).on(‘changed.owl.carousel’,function(event){var currentItem=event.item.index;var totalItems=event.item.count;if(currentItem===0){jQuery(‘.owl-prev’).addClass(‘disabled’)}else{jQuery(‘.owl-prev’).removeClass(‘disabled’)}
if(currentItem===totalItems-1){jQuery(‘.owl-next’).addClass(‘disabled’)}else{jQuery(‘.owl-next’).removeClass(‘disabled’)}})}})})